Sep 19
SF sees uptick in new HIV cases, especially among Black people and women
Liz Highleyman READ TIME: 5 MIN.
San Francisco saw a small increase in new HIV diagnoses last year, rising from an all-time low of 140 cases in 2023 to 146 cases in 2024, according to the latest HIV epidemiology annual report from the SF Department of Public Health, released Friday. The report shows an increase in diagnoses among Black people and women; in 2022, cases rose among Latinos.
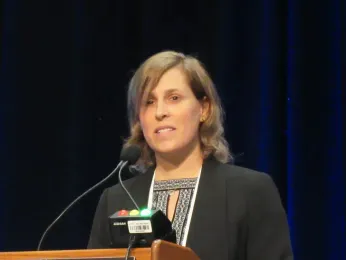
“The increase from 140 to 146 is not alarming – it’s a similar number. But what we want to be seeing is an ongoing decline in HIV infections,” Dr. Stephanie Cohen, director of DPH’s STI/HIV Prevention Branch, told the Bay Area Reporter in an interview. “What this says to us is that we need even more thoughtful, strategic, and intensive efforts to reach those who are still acquiring HIV to get to our Getting to Zero goals.”
The city's Getting to Zero program aims to reduce new HIV transmissions and HIV deaths by 90%, in addition to reducing stigma.
Last year’s 4.3% uptick follows two years of declines after a brief rise at the start of the COVID-19 pandemic. But overall, the long-term trend shows a decrease in annual diagnoses over the past two decades, down from 543 new cases in 2006.
“When you look back at the bigger picture, what we see is a pretty steep decline in HIV infections after the rollout of PrEP and the embrace of treatment as prevention, though progress has slowed in recent years,” Cohen said.
Overall, 94% of people diagnosed with HIV in 2024 were linked to care within one month and 79% achieved a viral load below 200 on antiretroviral treatment within six months. Among those diagnosed in 2023 – the latest year with complete follow-up data – 87% achieved viral suppression within one year.
A total of 11,552 San Francisco residents were living with diagnosed HIV at the end of 2024, according to the report. Thanks to effective treatment that enables HIV-positive people to live longer, 75% are now age 50 or older, and 29% are 65 or older.
“HIV diagnoses in San Francisco have declined by 53% over the past 10 years. This report shows that as a city, we must continue to remain persistent,” Health Director Daniel Tsai said in a statement. “HIV is a serious public health issue in San Francisco and across the country, and SF DPH is committed to the important work that helps prevent people from getting HIV and improving outcomes for people who are diagnosed with HIV.”
Disparities persist
As previously reported , Latino men had the highest HIV diagnosis rate for the first time in 2022, but last year Black men once again pulled ahead. There were 40 new cases among Black people in 2024 compared with 27 in 2023, a 48% increase. Latino people, however, accounted for the largest share of new diagnoses (32%), followed by Black people and white people (both at 27%). Asians accounted for just 14% of new diagnoses despite making up more than a third of the city’s population.
Also notable in this year’s report is the near doubling of HIV diagnoses among cisgender women, from 14 cases in 2023 to 26 cases in 2024, with the majority of cases among Black women. But still, gay and bisexual men accounted for 83% of all new diagnoses last year. Transgender women accounted for 6% of new cases, while trans men made up less than 1%.
While it is hard to draw conclusions about trends from small numbers, these figures reflect larger racial/ethnic and gender disparities across many health indicators, according to Cohen.
“We’re finding that women who are diagnosed with HIV in recent years experience a lot of intersecting vulnerabilities,” she said. “Homelessness, substance use, mental health issues, experiences of stigma and discrimination, and [lack of] access to care are particularly pronounced in that population, which is why we need wrap-around services that address social determinants of health.”
HIV diagnoses among homeless people decreased from 32 to 24 last year, making up 16% of new cases, down from 23% in 2023. However, the proportion of diagnoses among cisgender women experiencing homelessness was high. People who inject drugs accounted for 14% of cases.
“The fact that, overall, the proportion and number of new cases among people experiencing homelessness went down is certainly welcome,” Cohen told the B.A.R. “We have a lot of programs that are working to improve screening, prevention, and linkage to and retention in care for people experiencing homelessness, and I certainly hope that those programs are helping make a difference.”
That difference is reflected in improving care indicators for this population. The report shows that 88% of homeless people diagnosed in 2024 were linked to care within one month and 68% of those diagnosed in 2023 achieved a viral load below 200 within one year. While this is still well below the 91% viral suppression rate for people with stable housing, it reflects progress over time.
One reason for the improvement may be the advent of new tools, including long-acting injectable antiretrovirals for HIV treatment and prevention. ViiV Healthcare’s injectable cabotegravir plus rilpivirine (Cabenuva), administered once monthly or every other month, is the longest-acting treatment regimen, while cabotegravir alone (Apretude) is used for PrEP.
“For people experiencing homelessness who are living with HIV, we’ve found that long-acting injectables are often a preferred medication,” Cohen said. “The [Zuckerberg San Francisco General Hospital] Ward 86 program and its POP-UP clinic, in particular, has been very successful in providing long-acting Cabenuva for treatment of people experiencing homelessness and has had some excellent outcomes.”
Looking to the future
This 2024 epidemiology report does not yet reflect the effects of the Trump administration’s cuts to federal funding for HIV prevention, care, and treatment. Experts fear that these reductions will lead to a rise in new cases and poorer outcomes for people living with HIV. Earlier this month, advocates held a rally on Capitol Hill to protest pending cuts to HIV prevention, services, and research in the United States and worldwide.
On the other hand, the advent of twice-yearly PrEP could help finally end the epidemic if it’s accessible to those who need it most. Nearly two-thirds (63%) of HIV-negative gay and bi men seen at City Clinic were on PrEP in 2024, according to the report, but use lags among women and Black and Latino men. Longer-acting options could help close the gap.
The federal Food and Drug Administration approved Gilead Sciences’ lenacapavir (brand name Yeztugo) for HIV prevention in June. Two large trials showed that the injections given once every six months were 100% effective for young cisgender women in Africa and 96% effective for gay and bi men and gender-diverse people in the United States and six other countries.
The early rollout of twice-yearly PrEP is now underway in San Francisco. “At this point, we still have very small numbers of people who have been prescribed lenacapavir for PrEP, but we have a major focus on working to get it out into the community much faster than other PrEP tools have rolled out,” Cohen told the B.A.R.
“I think everyone in the HIV prevention world is very excited about having a medication that’s given just once every six months that is so highly effective at preventing HIV. That’s really a huge step forward,” she said. “There’s still more to learn about who is going to choose lenacapavir for PrEP, but we are quite excited that we have this new tool, and we are really hopeful that it will reinvigorate the progress that has slowed in recent years.”
The full report is here.
Updated, 9/20/25: This article has been updated to state that the current number of SF residents living with HIV is 11,552.


